As we explained in our last newsletter, diagnostic imaging tests can be a vital tool that helps doctors more clearly understand what’s happening in the body in order to reach or confirm a diagnosis. But simply because these tests are helpful does not mean they should be used at all times, or even frequently. For musculoskeletal disorders—like back, neck, and knee pain—imaging tests should be used when certain criteria are met, yet statistics on their use paint a much different picture.
The overuse of diagnostic testing for musculoskeletal disorders is part of a much larger trend in the healthcare industry. According to one article, about $800 billion of healthcare spending is spent on unnecessary diagnostic tests, procedures, and extra days in the hospital. For musculoskeletal disorders, back pain typically garners the most attention because it is so common and because it serves as one of the clearest examples of excessive diagnostic testing use.
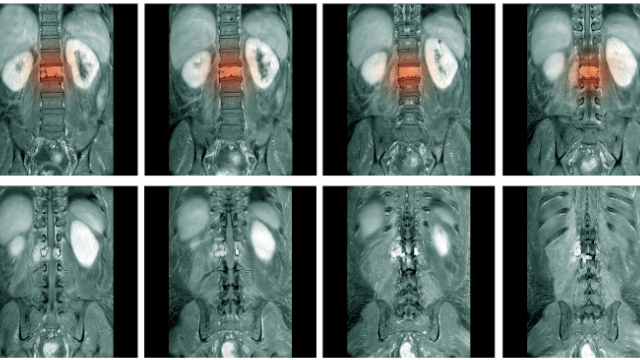
Low back pain is one of the most common overall ailments and will affect up to 80% of individuals at some point in their life. Imaging tests are only recommended when a “red flag” is present, which include signs of severe or worsening nerve damage, serious underlying problems like cancer or spinal infections, unexplained weight loss, loss of bladder or bowel control, and abnormal reflexes. If none of these red flags are present, an imaging test is not usually required, but many patients with back pain continue to have MRIs of their spine for one reason or another.
Despite the existence of guidelines that recommend against MRIs, except for in these rare cases, there is data that shows many patients with back pain are initially being prescribed diagnostic imaging tests without first attempting less expensive and less invasive treatments like physical therapy. In fact, one study estimated that the use of MRIs for low back pain increased by as much as 300% between 1994-2006. And while it may seem as if the overuse of these helpful tests is generally harmless, the inverse is actually true.
For starters, imaging tests—particularly MRIs and CT scans—are extremely expensive. The average cost of an MRI is $1,119, with some costing as much as $3,000, which is significantly higher than any other comparable countries. CT scans and X-rays also expose patients to potentially harmful levels of radiation that could otherwise be avoided. But perhaps most importantly, imaging tests can do more harm than good for many patients. This is because they don’t always identify the cause of patients’ pain—especially for low back pain—and often reveal “abnormalities” unrelated to the pain that may be misconstrued as a cause. An important study highlights why this is true, as it reviewed the MRIs and CT scans of more than 3,000 individuals with no signs of back pain. Results revealed the following:
- 20-year-olds: 37% had “disc degeneration” and 30% had “disc bulging”
- 50-year-olds: 80% had “disc degeneration” and 60% had “disc bulging”
- 80-year-olds: 96% had “disc degeneration” and 84% had “disc bulging”
These results show that disc degeneration and disc bulging are extremely common in most people without back pain, and the likelihood of having these “abnormalities” increases significantly with age. Therefore, many patients with back pain may be told that they have disc degeneration or disc bulging and believe this to be the reason for their pain, while the truth is that it is likely a sign of the natural aging process instead.
Another extremely unfortunate consequence of this testing is that many patients go on to receive invasive, dangerous, and expensive interventions based on the results of their tests, even if the procedure won’t actually resolve their pain. In our next newsletter, we’ll explore the repercussions of overusing diagnostic imaging tests in more detail and explain why this can all be avoided by seeing a physical therapist first.
